Rheumatoid Arthritis

Rheumatoid Arthritis
What is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an incurable, progressive autoimmune disease in which the body's immune system attacks the lining membrane of joints (synovium) and joint cartilage throughout the body. Rheumatoid Arthritis leads to thickening of the synovial membrane (which lines the joints) and an overproduction of synovial (joint) fluid. As a result, joints become painfully inflamed, swollen, and stiff. Rheumatoid Arthritis can be crippling. As a chronic and destructive disease, the damage to cartilage and other soft tissue can lead to permanent joint damage and progressive loss of mobility.
In addition to joint damage, Rheumatoid Arthritis can cause numerous their symptoms including chronic fatigue, anaemia, and weight loss.2 It can also have an effect on other tissues and organs, leading to complications with the lungs, heart, and eyes. Rheumatoid Arthritis is different from osteoarthritis, which is the more common form of arthritis, involving deterioration of joint tissue through wear and tear, usually among older individuals. Currently, there is no cure for Rheumatoid Arthritis - it is a lifelong condition.
Impact of Rheumatoid Arthritis
Rheumatoid Arthritis is wide-ranging, affecting the physical well-being and quality of life of over 500,000Australians, impacting the average life expectancy, shortening it by three to seven years. Women are twice of likely to develop Rheumatoid Arthritis, than men. The peak onset of Rheumatoid Arthritis is between 25 and 50 years of age - a time when people are most active in their workplace and in taking care of family and within 10 years of diagnosis, approximately 50% of people are unable to work full time.
Causes of Rheumatoid Arthritis
The causes of Rheumatoid Arthritis are unknown; however, it is known that genetic susceptibility, infections, hormones and environmental factors including smoking are risk factors for the disease.
Diagnoses of Rheumatoid Arthritis
Diagnosis of Rheumatoid Arthritis is not based on one conclusive diagnostic test; doctors must consider a number of criteria including the patient's history of signs and symptoms (often for several weeks), physical examination, and laboratory tests before a diagnosis of RA can be confirmed. The first symptoms that lead patients to go to see their doctor - joint pain, morning stiffness, and joint swelling - are often quite typical and can have many causes. This often starts in the finger joints and then spreads throughout the body. Early symptoms are then followed by deformities and rheumatoid nodules (lumps that develop under the skin at sites subject to mechanical strain). In conjunction with the clinical signs and symptoms of RA, blood tests and imaging techniques (x-rays, magnetic resonance, ultrasound) can provide evidence of acute joint inflammation and joint damage.
Early diagnosis and prompt use of effective treatments for Rheumatoid Arthritis are very important in order to minimise the potential for irreversible damage to the joints - up to 80% of people with Rheumatoid Arthritis have signs of permanent joint damage within the first two years of their disease. People with Rheumatoid Arthritis are often first seen or diagnosed by a primary care physician (general practitioner), so referral to a specialist (rheumatologist) within the first three months after diagnosis is critical to ensure appropriate and timely treatment.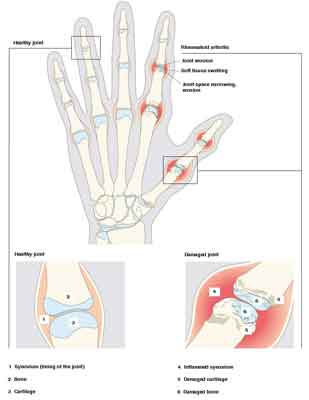 Treating Rheumatoid Arthritis
Treating Rheumatoid Arthritis
Rheumatoid Arthritis is a chronic autoimmune disease and requires lifelong treatment. Treatments for Rheumatoid Arthritis have advanced rapidly over the past few years, helping people achieve the ultimate goal of remission, which is the absence or significant reduction of symptoms like pain, stiffness, swelling and fatigue.
A variety of therapies exist today, which make it possible to take control of Rheumatoid Arthritis and improve quality of life, so there is little reason why most people with Rheumatoid Arthritis should suffer with progressive symptoms. Treatments work differently in each person and at different stages of the disease, so it is common for people with Rheumatoid Arthritis to try different treatment options as the disease changes. People who think their treatment is not working well enough should seek advice from their doctor.
Painkillers and anti-inflammatories are typically used to relieve mild symptoms of rheumatoid arthritis, such as pain, swelling and inflammation. Commonly used examples of painkillers include paracetamol and aspirin, which are administered in tablet or capsule form.
Non-steroidal anti-inflammatory drugs (NSAIDs) are used to reduce the inflammation, pain, and swelling associated with Rheumatoid Arthritis. Examples of NSAIDs include naproxen and ibuprofen. They are administered in tablet or capsule form.
Corticosteroids are also used to reduce inflammation. However, because of the side-effects of long-term use, they are typically only used for short periods or if someone is not responding to NSAIDs. Corticosteroids are administered as tablets, by self-injection, or by local (topical) application.
Disease-modifying anti-rheumatic drugs (DMARDs) slow the progression of the disease by suppressing the immune system. They are standard therapy for people at risk of joint damage and deformity. Most people with Rheumatoid Arthritis will be treated with a DMARD as a standard therapy option for the duration of their disease, either alone or in combination with another therapy (e.g. a biologic therapy). Common examples of DMARDs include methotrexate, hydroxycholoroquine, and leflunomide, which are administered as tablets or by self-injection.
Biologic therapies, which specifically target the proteins responsible for inflammation, have revolutionised the treatment of Rheumatoid Arthritis by offering benefits for people whose severe Rheumatoid Arthritis has not responded well to standard treatments. Biologic therapies work in different ways, but all block specific steps in the inflammation process. They are often prescribed in addition to DMARDs as treatment for patients with severe Rheumatoid Arthritis. Biologic therapies available in Australia for rheumatoid arthritis are:
IL-6 receptor inhibitor, e.g. tocilizumab. This biological treatment is administered by IV infusion under the supervision of a healthcare professional.
B and T cell-targeting biologics, include rituximab and abatacept.These are administered by IV infusion under the supervision of a healthcare professional.
 Monitoring Rheumatoid Arthritis
Monitoring Rheumatoid ArthritisPeople with Rheumatoid Arthritis have an important role in monitoring their condition and speaking openly with their doctor to ensure they receive the most from their therapy and take control of their disease.
Rheumatoid Arthritis Treatment: Actemra® (tocilizumab)
Actemra® (tocilizumab) now available for thousands of Australian's living with this incurable disease.
The first rheumatoid arthritis treatment designed to block the chemical messenger interleukin-6 (IL-6), which causes chronic inflammation, is now accessible to thousands of Australians living with this chronic and disabling inflammatory disease.
On 1st August, Actemra will be listed on the Pharmaceutical Benefits Scheme (PBS) for the treatment of severe, active rheumatoid arthritis in adults whose conventional treatments are no longer effective.
The treatment of rheumatoid arthritis has advanced rapidly with the introduction of biologic treatments, which have revolutionised the way people are treated.3 Actemra is a rapidly-acting biologic therapy that treats rheumatoid arthritis by attacking inflammation at its source. It targets IL-6, an important driver of the chronic inflammation, joint damage, pain, anaemia and fatigue experienced by people diagnosed with this painful autoimmune disease. People with rheumatoid arthritis have excessive amounts of IL-6 in their joints.
Rheumatologist at Royal Prince Alfred Hospital in Sydney, Associate Professor Peter Youssef said, "Thegovernment's decision to fund Actemra is welcome news for people with severe rheumatoid arthritis. Currently, many people with severe rheumatoid arthritis fail to respond to existing treatments and Actemra provides another alternative for people living with this disease."
"Rheumatoid arthritis is debilitating and causes crippling pain. With the advancement in treatment, patients have a chance to lead productive lives again and even be free from pain, stiffness, swelling and fatigue. Actemra is different to other treatments because it attacks the IL-6 chemical messengers responsible for causing chronic inflammation," said Associate Professor Youssef.
The ultimate treatment goal for people with rheumatoid arthritis is remission, which is the absence or significant reduction of symptoms. Remission can provide people with rheumatoid arthritis a chance to enjoy a life free of symptoms like pain, stiffness, swelling and fatigue, enabling a better quality of life. With the availability of a wider range of treatments, including biologics, remission is a real possibility for people with rheumatoid arthritis.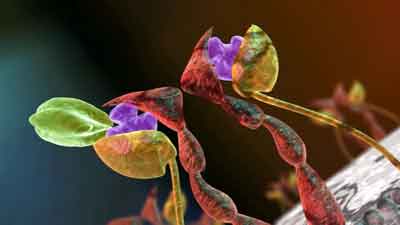 Actemra® Pharmaceutical Benefits Scheme (PBS) Listing
Actemra® Pharmaceutical Benefits Scheme (PBS) Listing
On 1st August, 2010 Actemra® will be listed on the Pharmaceutical Benefits Scheme (PBS) for the treatment of severe, active Rheumatoid arthritis in adults, either in combination with methotrexate or as monotherapy (where methotrexate is not tolerated) in patients who have failed to achieve an adequate response to previous therapy with two or more disease-modifying anti-rheumatic drugs (DMARDs) and who meet certain criteria.
To date, an estimated 34,000 people have been treated with Actemra globally, primarily for RA, but also for other autoimmune diseases. Nearly 500 Australian patients have been treated with Actemra for rheumatoid arthritis. Actemra has a well defined safety profile, which has been investigated in the largest phase III clinical development program in rheumatoid arthritis, involving more than 4,200 patients.
Like all effective treatments, Actemra has the risk of side effects. The most common adverse reactions for Actemra include upper respiratory tract infection, headache, high blood pressure and altered liver function (e.g. increase in ALT and AST enzymes). Other adverse reactions may include altered cholesterol levels, recurrence of underlying conditions (e.g. diverticulitis - inflammation in the lining of the bowel), and infusion reactions. Actemra should not be used in patients with active, severe infections.
Contact your healthcare professional or rheumatologist for further information and to discuss the best treatment option for you.

Interview with Maria Sciarrone
Maria Sciarrone was diagnosed with Rheumatoid Arthritis when she was just 36 years old.
Can you talk about your diagnoses?
Maria Sciarrone: As a sufferer of Rheumatoid Arthritis it is an increasingly common problem in our community and throughout the world. It has a significant impact on sufferers, their quality of life and insures chronic pain and disability. Most individuals with this arthritis condition experience loss of function, pain and stiffness and are dealing with a disease that is long lasting. I have spent 12 years in taking charge to know as much and to work with all doctors with different qualifications to treat this condition and what treatments can be helpful to each individual. Each of us would like to improve our quality of life and with the drugs available to us that proudly worked for me as well as others with compelling results. I hope I can inspire all those who suffer from Rheumatoid Arthritis that there is hope and if they go out and see their doctors and make some enquiries, I'm sure there will be some wonderful and compelling results. It is a matter of trying and seeing what suits the individual. As for myself, I can say that the results have been very compelling.
Prior to your diagnoses did you know anyone who had Rheumatoid Arthritis?
Maria Sciarrone: No, not at all. I was in shock. I hadn't heard anything of this condition before, it hit me really hard because it is something you see a lot of the elderly having, you don't think it's some thing that can affect anybody.
What symptoms did you have?
Maria Sciarrone: Basically I had lots of pain in my fingers in my joints and in my wrist, shoulders, knees and hips, it was like a ache of bad pain, all over my body. I also felt very stiff in the morning, when I got out of bed, I was unable to move freely and I was very immobile. It got to the point, where, I was working at the time, I'd have to ring up work and say "look I can't come in today; I'm really not feeling well". I didn't know if I was coming up with the flu or what. I ended up going to see the GP and I had some blood tests and sure enough, I was diagnosed with Rheumatoid Arthritis.
How did you life change when you were diagnosed with Rheumatoid Arthritis?
Maria Sciarrone: It totally changed. I couldn't go to work, I was so immobile and so sick I ended up in hospital for three weeks. I was bed-ridden and I couldn't walk around, even coming out of the hospital and I had to be taken around in a wheelchair, by my husband, to the shops. I had so much swelling in all my joints, I couldn't shower, by myself and I needed help to do everything. I was lucky I had my daughter and my husband, I had a double storey house and I had to live downstairs, because I couldn't walk upstairs.
You have three children, how did they cope when you were diagnosed with Rheumatoid Arthritis?
Have you been able to go back to work?
Maria Sciarrone: I still do a little bit of hairdressing from home; I now am a part-time sales assistance in a retail store. It took me a long time before I could go back to work because I had to trial, over a number of years, different medications before I got onto Actemra. Therefore I didn't have 100% stability in my health because it varied, daily. Some days I'd chronically be in bed, really ill and there were days were I couldn't bend down or I couldn't walk or drive. I am back at work, part time.
 You have been in remission for four years, how does Rheumatoid Arthritis affect your daily life?
You have been in remission for four years, how does Rheumatoid Arthritis affect your daily life? Maria Sciarrone: Nothing, it doesn't affect my life whatsoever now, which is fantastic! Now I can do everything, it is great; it has taken a lot of pressure off at home as well because now I don't have to rely on family members to do things for me. I can do all the things I always used to do before, like cutting the lawn, jet skiing and kicking the football with my son at the football oval. All the things I couldn't do, I now can do, which is wonderful, I can actually do my shopping, without having to rely on anyone to help me. Actemra changed my life tremendously.
How long did it take for you to find the right treatment for your Rheumatoid Arthritis?
Maria Sciarrone: I tried quite a lot of different treatments; I think I would have gone through at least ten different treatments before I ended up getting onto Actemra.
Actemra is now available on the Pharmaceutical Benefits Scheme, how does this help you and other Rheumatoid Arthritis sufferers?
Maria Sciarrone: It is wonderful. It is fantastic, it makes my whole life complete knowing that it has been accepted on PBS and is now affordable, not just for myself but for everybody. It is going to make my life so much better and easier. It is wonderful.
I highly recommend Actemra, it is no good staying home thinking 'it's just my arthritis'. Yes, we have to deal with it because it is there with you for life but if you can give yourself the quality of life where you can do normal activities and feel pain free, why not?
It has done an amazing turn around and now I don't have to sell my house, because we thought about selling our home because it was double storey. Now I can go up the stairs and go bike riding. It is fantastic to think that with this I can move freely and be pain-free and not wake up in the morning feeling totally stiff and immobile and restricted on how I could move and what I could do. I feel like I have as healthy of a life as anyone else, I know. It has been a big turn around for me.
I always spread the news and try to speak to lots of people about Actemra, because I highly recommend it. I urge a lot of people, as it is quite distressing having Rheumatoid Arthritis, it certainly impacts on your life. Having to have the infusions, once a month, like I do, is fantastic, giving my life a huge turn around in everything I do. I can even dance now and not worry about my hips or knees going on me!
When I was diagnosed it hit me like a bomb, at the time when I was first diagnosed, my baby, young Joseph was only about 12 months, and I had to rely on my husband and the children to help with him. My oldest, was playing second Mum. I am very fortunate to have my family and a doctor as wonderful has Profession Stephen Hall who is an expertise in treating people with this condition. It is amazing how he has comforted people's lives; he is one in a million.
Going from such a debilitating condition to having a normal and healthy life, is wonderful.
MORE
- Cold Sores
- Glandular Fever
- FAQ About Irritable Bowel Syndrome
- February is Ovarian Cancer Awareness Month
- Help find answers for Herpes
- National Eczema Awareness Week
- Claire Naffah It's Dementia
- Skin Cancer and Melanoma
- Treatment for Early-stage Breast Cancer
- Structured Reporting for Cancer Patients
- Tuberculosis