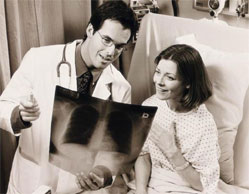
Are you afraid of Mammography and diagnostic breast interventions?
Women are generally tough, strong creatures who have a high tolerance for pain. They uncomplainingly go for pap smears, go through labour pain, have much less of an aversion to needles than the masculine sector of the population and yet when it comes to mammography, they complain in an uncharacteristically volatile manner.
My qualifications to write this article are that I wear three hats, that of radiographer/mammographer, psychologist as well as patient who has undergone all of the diagnostic breast interventions. I speak from professional as well as personal experience and one of the big questions I have wondered about is this question of "why the enormous fuss made about going for a mammogram?"
As a psychologist I know that we often find uncontrollable and unpredictable events really frightening. My theories about explaining the fuss is that it is hardly the pain factor at all but rather our anxiety that is linked to the pain which makes it such a fearful experience for some. For some it may be that the breast is a symbol of love and nurturing and it is very rude to treat this part of a woman's body in such a harsh, callous manner. For some they may feel genuine pain because they have particularly sensitive breasts but, in my experience, they are a small minority. I also believe that male doctors tell their patients that it is very painful because they imagine how it would feel to have their own genital appendages compressed between two plates! They have nothing else to go on.But mostly I believe that it is feared because of the catastrophic consequences of finding out that one has the unmentionable- a breast cancer!
The only method currently appropriate for screening for breast cancer is mammography. Screening mammography has been shown to reduce mortality by 30-50%, through improved early detection. Mammography has a sensitivity of 90%. About 10% of all cancers of the breast are not detected initially by mammography. Therefore a negative mammogram does not exclude breast cancer in the presence of clinical symptoms. Mammography is highly sensitive for detecting cancers that contain micro-calcifications. These micro-calcifications look like grains of salt on the mammogram and occur in up to 50% of all cancers. Those cancers which contain micro-calcifications account for 30-40% of invasive cancers and 90% of non-invasive cancers. The very high sensitivity for detecting non-invasive cancers of the breast that contain micro-calcifications is one of the major benefits of mammography as these have an excellent prognosis and are curable with appropriate surgery.
Having a mammogram can save your life! It is the aim of this article to explain the diagnostic procedures from a layman's point of view because it is my hope that those of you who resist having regular mammograms because you fear them, will change your mind if you are better informed. Mammography does not hurt that much. Most people find it a bit uncomfortable. And each of the exposures last for a few seconds!
Knowledge is power and puts you more in control of the situation. If you know what to expect, you will feel much more in control and are in a position to put some coping strategies into place.
Why is mammography the only way to detect an early breast cancer?
65% of diagnosed breast cancers diagnosed from mammography are intraductal. This means that the cancer cells are completely contained in the milk ducts and have not spread into the surrounding breast tissue. As long as the cancer cells have not become invasive, they cannot spread in the blood and lymphatic system and they therefore cannot metastasise to other parts of the body. A palpable cancerous breast lump is felt when this invasion of the surrounding breast tissue has occurred. Mammography is able to detect the presence of intraductal carcinoma because of the presence, shape, size and density of micro-calcifications which are deposited between the cells which line the walls of the ducts. These are in the order of millimetres, occur long before a lump is formed and are not detectable in any way other than mammography.
What does ultrasound of the breast show?
Ultrasound uses sound waves rather than X-rays to image the breast. It is a diagnostic tool used as a problem solver to characterise a lump that is palpable or detected on mammography. This method is able to determine whether the lump is solid or cystic (fluid filled). Simple cysts are common and are benign. If however it is found to be solid, then further procedures are required in order to arrive at a clear diagnosis.
Ultrasound does not hurt at all. The sonographer uses gel and a transducer to scan the breast which is imaged on what looks like a TV screen.
Fine Needle Aspiration (FNA) under X-ray guidance
If there is a density on the mammogram or a collection of micro-calcifications, then further investigations have to be performed in order to establish whether or not there is cause for concern. An area of concern, which can only be seen on a mammogram and which is not palpable, is then able to be localised, within a millimetre of accuracy, by means of stereotactic X-ray guided fine needle aspiration of the breast. Some practices have equipment which involves sitting very still whilst the breast is held immobile by a compression plate so that a needle can be introduced into the area of concern. The radiologist removes aspirates or samples of tissue from the area when the needle has been guided accurately into the area of concern by means of this highly sophisticated technique. A pathology technician is present who takes smears of the aspirate to the pathology department for later analysis by the pathologist.
In my experience (and I have had many FNA's) the procedure is painless. The radiologist injects local anaesthetic into the area which may sting a little. Afterwards one can feel the pressure of the needle but that is all. Sometimes the area of concern is very deep and the local anaesthetic is not as effective. The pain factor is minimal. The biggest problem is sitting with one's breast clamped in a compression device for a long period of time. Sometimes one's neck gets in the way and makes it awkward but the more relaxed one is and the better position one is sitting in from the outset, the less of a problem this is.Other practices have a set-up where one lies face down on a bed and the radiologist and mammographer work underneath one (as if the patient is a motor car that has been jacked up hydraulically and the mechanics do their thing undernealth!). One's breast is positioned through an opening in the bed and this is much easier on the neck and it is also much easier to maintain immobility. The technique is otherwise the same.
FNA under Ultrasound guidance
This is a really easy procedure to go through as one simply lies comfortably on a bed on one's back and the radiologist introduces a needle into the area of concern which is guided by the ultrasound transducer and imaged to be in the correct position on the monitor. As above, aspirates are taken and sent to pathology and the radiologist uses local anaesthetic. I have had lots of these sorts of FNA's and found them to be one hundred percent painless.
Core Biopsy
A core biopsy is done in the same way as the FNA either with X-ray or Ultrasound guidance but a biopsy "gun" is used instead of the needle. This takes a thicker core of breast tissue and is more sensitive and specific than FNA. This is particularly useful for assessing the significance of micro-calcifications which are detected on mammography. Core biopsies are also used to further assess lumps that have already been subjected to FNA where insufficient or non-diagnostic material has been obtained.
Mammotome
This is the most sophisticated of all the diagnostic techniques and the closest one can come to having an excision biopsy without surgery. As far as I know, this technique is only used in one practice in Perth. This procedure uses a larger needle to obtain larger core biopsies using a gentle vacuum suction technique. Digital imaging is used to guide the needle into position. The procedure is done in the same way as an X-ray guided FNA lying prone on the bed.
Hook-wire localisation
When it has been established that there is an abnormal area in the breast that cannot be felt but which can be seen on mammography or ultrasound, then the radiologist introduces a hook-wire into the abnormal area using mammography or ultrasound guidance. This is then used by the surgeon as a pathway to the lesion, so that he or she can excise the area with accuracy and good margins. In my experience this is fairly painless but a bit creepy thinking about having a wire inserted into one's breast.
Strategies
A mammogram is only as good as the equipment available, the skill of the technician and the ability of the radiologist. Find out the best place to go for the examination.
If you are nervous about any of the procedures tell the technician and ask for explanations of what exactly to expect.
If you fear pain, while the procedure is underway keep asking yourself "what is the evidence that this is painful?" Scan your body for evidence of pain in your mind's eye. It is more likely that because you are tense and hypervigilant for signals of pain, that you are over reacting to feelings of pressure or light discomfort.
If you are still nervous and feeling tense and shaky, practice focussing on breathing in and out slowly. It you are paying attention to breathing, you cannot pay attention to the procedure at the same time. Breathing and focussing in this way help as distraction as well as stopping you from hyperventilating and causing sensations of panic.
Some people find it helpful to imagine they are in a place that is full of peace, beauty and tranquillity. Others find it helpful to engage in conversation unrelated to the procedure.
Find out what works for you and practice it.
If you have no family history of breast cancer you should have a mammogram once every second year after the age of 40 and if you do have a family history, you should be having them annually. It is imperative that you always take your previous mammograms with you as the Radiologist will want to compare the current mammogram with your previous ones to look for subtle changes. This can markedly improve accuracy of mammography.
- Bev Green
My qualifications to write this article are that I wear three hats, that of radiographer/mammographer, psychologist as well as patient who has undergone all of the diagnostic breast interventions. I speak from professional as well as personal experience and one of the big questions I have wondered about is this question of "why the enormous fuss made about going for a mammogram?"
As a psychologist I know that we often find uncontrollable and unpredictable events really frightening. My theories about explaining the fuss is that it is hardly the pain factor at all but rather our anxiety that is linked to the pain which makes it such a fearful experience for some. For some it may be that the breast is a symbol of love and nurturing and it is very rude to treat this part of a woman's body in such a harsh, callous manner. For some they may feel genuine pain because they have particularly sensitive breasts but, in my experience, they are a small minority. I also believe that male doctors tell their patients that it is very painful because they imagine how it would feel to have their own genital appendages compressed between two plates! They have nothing else to go on.But mostly I believe that it is feared because of the catastrophic consequences of finding out that one has the unmentionable- a breast cancer!
The only method currently appropriate for screening for breast cancer is mammography. Screening mammography has been shown to reduce mortality by 30-50%, through improved early detection. Mammography has a sensitivity of 90%. About 10% of all cancers of the breast are not detected initially by mammography. Therefore a negative mammogram does not exclude breast cancer in the presence of clinical symptoms. Mammography is highly sensitive for detecting cancers that contain micro-calcifications. These micro-calcifications look like grains of salt on the mammogram and occur in up to 50% of all cancers. Those cancers which contain micro-calcifications account for 30-40% of invasive cancers and 90% of non-invasive cancers. The very high sensitivity for detecting non-invasive cancers of the breast that contain micro-calcifications is one of the major benefits of mammography as these have an excellent prognosis and are curable with appropriate surgery.
Having a mammogram can save your life! It is the aim of this article to explain the diagnostic procedures from a layman's point of view because it is my hope that those of you who resist having regular mammograms because you fear them, will change your mind if you are better informed. Mammography does not hurt that much. Most people find it a bit uncomfortable. And each of the exposures last for a few seconds!
Knowledge is power and puts you more in control of the situation. If you know what to expect, you will feel much more in control and are in a position to put some coping strategies into place.
Why is mammography the only way to detect an early breast cancer?
65% of diagnosed breast cancers diagnosed from mammography are intraductal. This means that the cancer cells are completely contained in the milk ducts and have not spread into the surrounding breast tissue. As long as the cancer cells have not become invasive, they cannot spread in the blood and lymphatic system and they therefore cannot metastasise to other parts of the body. A palpable cancerous breast lump is felt when this invasion of the surrounding breast tissue has occurred. Mammography is able to detect the presence of intraductal carcinoma because of the presence, shape, size and density of micro-calcifications which are deposited between the cells which line the walls of the ducts. These are in the order of millimetres, occur long before a lump is formed and are not detectable in any way other than mammography.
What does ultrasound of the breast show?
Ultrasound uses sound waves rather than X-rays to image the breast. It is a diagnostic tool used as a problem solver to characterise a lump that is palpable or detected on mammography. This method is able to determine whether the lump is solid or cystic (fluid filled). Simple cysts are common and are benign. If however it is found to be solid, then further procedures are required in order to arrive at a clear diagnosis.
Ultrasound does not hurt at all. The sonographer uses gel and a transducer to scan the breast which is imaged on what looks like a TV screen.
Fine Needle Aspiration (FNA) under X-ray guidance
If there is a density on the mammogram or a collection of micro-calcifications, then further investigations have to be performed in order to establish whether or not there is cause for concern. An area of concern, which can only be seen on a mammogram and which is not palpable, is then able to be localised, within a millimetre of accuracy, by means of stereotactic X-ray guided fine needle aspiration of the breast. Some practices have equipment which involves sitting very still whilst the breast is held immobile by a compression plate so that a needle can be introduced into the area of concern. The radiologist removes aspirates or samples of tissue from the area when the needle has been guided accurately into the area of concern by means of this highly sophisticated technique. A pathology technician is present who takes smears of the aspirate to the pathology department for later analysis by the pathologist.
In my experience (and I have had many FNA's) the procedure is painless. The radiologist injects local anaesthetic into the area which may sting a little. Afterwards one can feel the pressure of the needle but that is all. Sometimes the area of concern is very deep and the local anaesthetic is not as effective. The pain factor is minimal. The biggest problem is sitting with one's breast clamped in a compression device for a long period of time. Sometimes one's neck gets in the way and makes it awkward but the more relaxed one is and the better position one is sitting in from the outset, the less of a problem this is.Other practices have a set-up where one lies face down on a bed and the radiologist and mammographer work underneath one (as if the patient is a motor car that has been jacked up hydraulically and the mechanics do their thing undernealth!). One's breast is positioned through an opening in the bed and this is much easier on the neck and it is also much easier to maintain immobility. The technique is otherwise the same.
FNA under Ultrasound guidance
This is a really easy procedure to go through as one simply lies comfortably on a bed on one's back and the radiologist introduces a needle into the area of concern which is guided by the ultrasound transducer and imaged to be in the correct position on the monitor. As above, aspirates are taken and sent to pathology and the radiologist uses local anaesthetic. I have had lots of these sorts of FNA's and found them to be one hundred percent painless.
Core Biopsy
A core biopsy is done in the same way as the FNA either with X-ray or Ultrasound guidance but a biopsy "gun" is used instead of the needle. This takes a thicker core of breast tissue and is more sensitive and specific than FNA. This is particularly useful for assessing the significance of micro-calcifications which are detected on mammography. Core biopsies are also used to further assess lumps that have already been subjected to FNA where insufficient or non-diagnostic material has been obtained.
Mammotome
This is the most sophisticated of all the diagnostic techniques and the closest one can come to having an excision biopsy without surgery. As far as I know, this technique is only used in one practice in Perth. This procedure uses a larger needle to obtain larger core biopsies using a gentle vacuum suction technique. Digital imaging is used to guide the needle into position. The procedure is done in the same way as an X-ray guided FNA lying prone on the bed.
Hook-wire localisation
When it has been established that there is an abnormal area in the breast that cannot be felt but which can be seen on mammography or ultrasound, then the radiologist introduces a hook-wire into the abnormal area using mammography or ultrasound guidance. This is then used by the surgeon as a pathway to the lesion, so that he or she can excise the area with accuracy and good margins. In my experience this is fairly painless but a bit creepy thinking about having a wire inserted into one's breast.
Strategies
A mammogram is only as good as the equipment available, the skill of the technician and the ability of the radiologist. Find out the best place to go for the examination.
If you are nervous about any of the procedures tell the technician and ask for explanations of what exactly to expect.
If you fear pain, while the procedure is underway keep asking yourself "what is the evidence that this is painful?" Scan your body for evidence of pain in your mind's eye. It is more likely that because you are tense and hypervigilant for signals of pain, that you are over reacting to feelings of pressure or light discomfort.
If you are still nervous and feeling tense and shaky, practice focussing on breathing in and out slowly. It you are paying attention to breathing, you cannot pay attention to the procedure at the same time. Breathing and focussing in this way help as distraction as well as stopping you from hyperventilating and causing sensations of panic.
Some people find it helpful to imagine they are in a place that is full of peace, beauty and tranquillity. Others find it helpful to engage in conversation unrelated to the procedure.
Find out what works for you and practice it.
If you have no family history of breast cancer you should have a mammogram once every second year after the age of 40 and if you do have a family history, you should be having them annually. It is imperative that you always take your previous mammograms with you as the Radiologist will want to compare the current mammogram with your previous ones to look for subtle changes. This can markedly improve accuracy of mammography.
- Bev Green
MORE
- Menstrual Period Management
- The Secret to Weight Loss
- Feeling The Pain: How To Tackle Period Pain
- Period Pain and How to Survive It
- Gender Specific Medicine
- Helping Women To Start Those 'Difficult'...
- Michelle Boyd Ellura Interview
- Menopause Does Not Protect Women From Cervical...
- Five Ways to Balance Hormones
- Do You Really Know What Is Going On Down There?
- Do You Know Your Breasts?
- Dr. Stan Goldstein Sexual Health Choices Interview
- Breast Health Decision Question and Answers
- Breast Cancer Treatment Impacts Patients' Sex...
- Bladder Weakness More Common Than Hay Fever
- Belinda Reynolds How To Manage UTI's Naturally...
- Treat Bones Like Breasts
- Mammogram Technology
- Soodox for Women
- Chlamydia Most Commonly Reported STI In Australia
- Time For Reflection Is Great For Mental Health